Making the Match: An Interview with Dr. Donna L. Lamb
Published March 04, 2021
2021
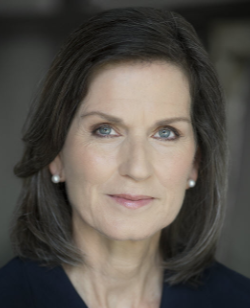 Donna L. Lamb, DHSc, MBA, BSN, has led the National Resident Matching Program (NRMP) as president and CEO since October 2019. The NRMP, or The Match, is a private, non-profit organization that uses a computerized mathematical algorithm to fill training positions available at US teaching hospitals. Research on the NRMP algorithm was a basis for awarding the 2012 Nobel Prize in Economic Sciences.
Donna L. Lamb, DHSc, MBA, BSN, has led the National Resident Matching Program (NRMP) as president and CEO since October 2019. The NRMP, or The Match, is a private, non-profit organization that uses a computerized mathematical algorithm to fill training positions available at US teaching hospitals. Research on the NRMP algorithm was a basis for awarding the 2012 Nobel Prize in Economic Sciences.
With Match Week quickly approaching, AACOM spoke with Dr. Lamb about her expectations for this year’s Match, her connections to the osteopathic community, and her vision for leading the organization into the future.
The answers below have been edited for brevity and clarity.
Q: Medical students will learn whether or not they matched at 11:00 AM ET on March 15, the first day of Match Week. If a student doesn’t match or partially matches, what can they expect throughout the Supplemental Offer and Acceptance Program (SOAP) process?
Dr. Lamb: For those who aren’t aware, SOAP is an entirely different process from The Match and does not use The Match algorithm to make a placement. Rather, it allows programs to receive applications, reach out and speak directly to unmatched or partially matched applicants and make offers in each of the SOAP rounds. Unlike the algorithm, SOAP applicants have the option to accept, decline or let an offer pass. If applicants accept, the agreement is binding. If they decline an offer or let it pass, they move on to the next SOAP round.
It’s important to note that SOAP is a stressful time for both applicants and programs. Applicants who enter the SOAP should expect to turn to their school advisors, mentors and other support systems to manage any disappointment they may be feeling and determine their strategy for approaching applications, keeping in mind SOAP’s rules to maintain equity. Once an applicant submits their SOAP applications, they may not reach out to any programs until the programs reach out to them, so once they apply, applicants should take a breath, wait until a program reaches out, and then they can pick up the phone, call the program and move forward with scheduling an interview.
Q: What was the rationale for adding a fourth SOAP round for this year’s Match? What are your general expectations for SOAP this year, and do they reflect larger trends that suggest an increase in SOAP participation? If so, why do you think these trends are occurring?
A: The rationale to add the fourth round of SOAP was two-fold. Reason one was that, at the end of SOAP last year, we had more positions unfilled than we typically would, about 40 more than normal, and we didn’t know why, although the COVID-19 pandemic suddenly threw everything into chaos. The United States declared a public health emergency on March 13, and Match Week started on March 16, so within a span of three days, programs were asking themselves, can we fill our positions, are we prepared to be able to interview, and will international medical graduates (IMGs) be able to get here? Not every program enters their unfilled positions in SOAP, and some decided to pull back and let their positions remain unfilled. Reason two was that we were unsure what would happen this year, not knowing how long the pandemic will last. This also raised questions about recruitment patterns and visa, exam and graduation issues. To provide optimal opportunities for applicants, we decided to extend the SOAP.
This year, we expect more people to enter SOAP because we have more applicants. As of March 1, there are 47,398 active registrants, which is about 8.2 percent higher than last year. Of these, 7,180 are osteopathic candidates, who, along with allopathic candidates, are vying for a total of 38,197 available positions, up from about 2.5 percent over last year. In terms of my general expectations, and this is pure speculation because I won’t know for certain until The Match actually runs, I don’t expect to see substantial changes in the DO and MD seniors match rate. I have some concerns about whether we will see a decrease in match rates for US and foreign IMGs due to the pandemic and changing pathways for Educational Commission for Foreign Medical Graduates (ECFMG) certification, along with their ability to get visas, but I don’t expect to see substantial changes in overall match rates for DO and MD seniors.
Q: Students have submitted their Rank Order Lists (ROLs) and are awaiting their results. Aside from running the algorithm, what is the NRMP busy doing between now and Match Week?
A: I can assure you the NRMP has been and will remain very busy. Applicants are submitting their ROLs earlier in the process than normal, which I think is amazing because it alleviates some concerns over lists being submitted on time. Currently, The Match operations staff is working to verify the eligibility of all the applicants. Even though applicants are registered and verified by their medical school and the NRMP makes sure IMGs have their ECFMG certifications, NRMP verifies and reverifies all data because things might have changed since applicants were first registered. NRMP operations staff also works with IT to structure the testing of The Match processes before we run the algorithm, and once we run the algorithm, we review the results to make sure it worked the way it’s supposed to, especially for those with more difficult Match lists, such as couples and programs with reversions. NRMP’s research team is also setting up all the reports that will become available, including the SOAP unfilled programs list, and the Results and Data Book with all Match data. This year we have a much shorter time between the ROL certification deadline and The Match, so the team is pretty busy!
Q: You received a Doctorate in Health Sciences with a concentration in Leadership and Organizational Behavior from A.T. Still University (ATSU), the founding institution of osteopathic healthcare. Can you describe how your experience at ATSU prepared you for leading the NRMP, particularly as we enter the second year of the fully implemented single graduate medical education (GME) accreditation system for DOs and MDs?
A: Going back for your doctorate allows you to expand your understanding of your worldview in general. My advisor was Dr. Joan Leafman, and she always pushed us to think outside of what we were reading. She had this wicked red pen that forced you to step back and think much more critically about what you were doing, beyond just completing an assignment. The education itself obviously prepares you to be more methodical and research oriented as you approach your work, especially your leadership and your organizational behavior. ATSU also allows you to bring real-world concerns and real-world projects into your doctorate program. When I began that program, I was working at Advent Health in Orlando, and was able to talk through programmatic GME issues with ATSU’s osteopathic faculty to better understand the differences between the allopathic and osteopathic training program experience. I moved into the Accreditation Council for Graduate Medical Education (ACGME) before completing my doctorate, and again, it increased my awareness of the differences and similarities between the DO and MD training communities, which also helped shape my perspective as we moved into the single accreditation system.
Q: You have been deeply engaged in the transition to a single GME accreditation system while at the ACGME serving as the Executive Director of Surgery, Plastic Surgery and Thoracic Surgery. Having overseen the first single match, what are you most proud of about the creation of this single system?
A: I should clarify that we began transitioning to the single match in 2016, before I arrived at the NRMP. Last year’s Match was the first fully implemented single match, so, really, we should credit Mona Signer, who is the prior NRMP president and CEO, and the executive leadership team, because they are the ones who carried the water on the development that got us here.
With that being said, what I am most proud of are the relationships and friendships I’ve made in the osteopathic community leading up to this transition. It was a very stressful time, and I’m proud of the trust the osteopathic community placed in me. It wasn’t easy for surgical specialties, especially, to become accredited because the surgical review committees are very critical of program structure and work to verify everything is in place before a program opens. Building relationships and trust allowed us to have some difficult conversations and work together to figure out how programs could meet the new requirements and become successfully accredited. It took a lot of work, but the community was very conscientious and understanding of what we needed to do and was very willing to collaborate. I’m proud of these relationships and think they will serve us well in the long run. Some of these folks, and AACOM’s President and CEO Dr. Cain is one, are people I know I can turn to and ask questions of to constantly make improvements, which is important, because the only way we can move forward together is through trust.
Q: AACOM recently honored Black History Month and remains committed to striving for diversity, equity and inclusion within all aspects of osteopathic medical education. The NRMP has committed to its mission and responsibility to provide a matching process that is fair, efficient, transparent and reliable. Can you describe how The Match algorithm works to ensure equity?
A: The algorithm itself creates order out of the chaos of offering and accepting positions, but it does not ensure diversity, equity and inclusion (DEI) in the way we normally think about it. One of the issues I’ve been discussing with the NRMP Board is the fact that, presently, the NRMP doesn’t collect any data not needed for running the algorithm, including race, gender, etc., so the system is blind as to how some of these factors may affect ranking and matching behaviors and patterns. For example, if there are only a few Black female medical residents in a particular specialty, we don’t know if it’s because Black female students aren’t selecting that specialty, or because the specialty programs aren’t selecting Black female students. Because of this, the NRMP Board in its January meeting decided that it will begin collecting demographic data for the purpose of doing the research to better understand these patterns.
The end of NRMP’s mission statement is about providing data and analysis, and frankly, we’re not providing an analysis right now. We’re not analyzing our ranking and matching data in the broad spectrum of DEI, or patterns within a specialty, but we are beginning to program our system to collect that information, which will help the medical education community better understand what is, right now, somewhat anecdotal. Before we made this decision, we did a call for public comment—the first time the NRMP had done that—because this data can be sensitive and uncover uncomfortable patterns, but the community, and the learners particularly, were very supportive. We expect that this data will be part of the registration for the next Main Residency Match, with the understanding that it will take a few years to collect enough data to draw meaningful results, especially ones that are not skewed by the pandemic. However, data is only one piece of puzzle, because issues such as clinical exposure, equity in modeling and interviews, and program transparency all affect equity. We are a member of, and working with, the Coalition for Physician Accountability, which is looking at the UME-GME transition and making recommendations to various stakeholders about how to address pain points in the process, but there needs to be more. We also need to be working with specialty societies, programs, learners, and organizations outside of medicine, too. So, to answer the question, the algorithm assures order from chaos and the NRMP is working to advance DEI through research and partnership.
Q: Looking toward the future, what do you hope to accomplish through the NRMP in the years ahead?
A: We are really looking at how we can improve processes for our stakeholders all the way around. Implementing innovative Match processes that are intended to help relieve pain points in the system is what I really hope to accomplish with the NRMP going forward. I can’t identify exactly what these are right now because we are still doing that work, but improving processes is a major goal.
Q: What advice would you share with current or future medical students preparing to match into residency training?
A: I’ll tell you what I used to tell the residents. Find a mentor you can trust and talk to openly, honestly and frequently. It shouldn’t be an event to talk to your mentor, they should be someone you can bounce ideas off every day and not be afraid to be honest with. Also, be honest with yourself about who you are, what you are and what you want for your future. Take the long, 10–20-year view. Today is most likely painful. You’re a student entering your first “job,” so-to-speak, and you’re newly accountable for the lives of your patients. Recognizing that it’s stressful now, but staying focused on your long-term goals, will help you get through what you’re experiencing at this stage of your medical career.Most importantly, even though this advice is not unique, is to take time for yourself. You are entering a tough profession that requires everything of you, intellectually, emotionally and physically. The job comes with lots of criticism, highs and lows, and situations and surroundings most people haven’t dealt with before. You will need to try to deal with your own fears and concerns while also needing to be fully present to take care of your patients and their families. You really can’t take care of others if you’re not well. Finally, be open to new things and remember that a closing door means another will open, and it may be something you never imagined for yourself but is exactly what you wanted. Take the open doors when they arise, stay true to who you are and allow yourself to think and dream, and again, take care of yourself.
