From Simulation to Specialty: Introducing Osteopathic Medical Students to Gastroenterology
Published February 18, 2026
Inside OME

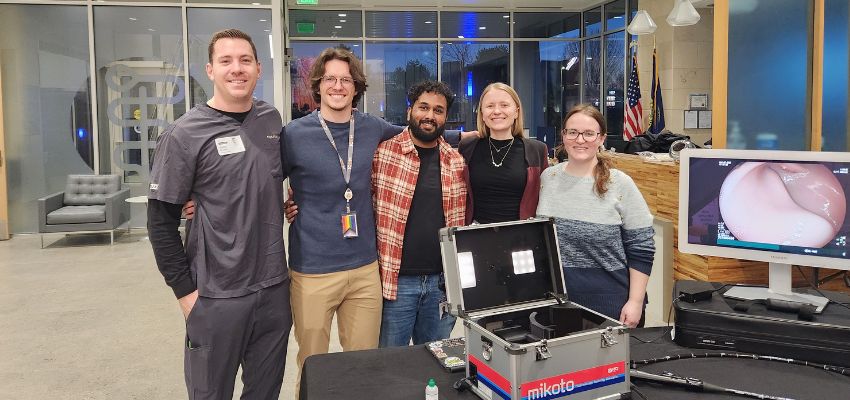
By ICOM Gastroenterology Interest Group leaders (from left to right) Juliana Madej, OMS II, president; Hagen Schultz, OMS II, vice president; Allison Gronli, OMS II, secretary; Murali Bollampally, OMS II, treasurer
The Gastroenterology Interest Group at the Idaho College of Osteopathic Medicine (ICOM) proudly hosted its first hands-on endoscopy simulation event, “Scope It Out! A GI Endoscopy Simulation Experience,” in collaboration with Fujifilm Endoscopy. This opportunity provided medical students with an early introduction to the dynamic field of gastroenterology and highlighted the essential role that endoscopy plays in both diagnosis and treatment.
Recent analyses of gastroenterology fellowship match trends demonstrate that U.S. osteopathic medical graduates represent the lowest proportion of matched trainees over the past 15 years when compared with allopathic and international medical graduates.¹ This disparity suggests potential gaps in early exposure to the specialty, understanding of gastroenterology or perceptions of the field among osteopathic medical students.
Specialty and subspecialty choice is influenced by multiple factors, including mentorship, early clinical exposure, research opportunities, perceived scope of practice and alignment with personal interests and values.²-⁶
Simulation-based educational interventions have been shown to positively influence medical student perceptions and interest across several procedurally oriented specialties, including surgical and interventional fields.⁷-⁹ Although endoscopy simulation has traditionally been used in fellowship training to support skill acquisition in a low-risk environment, emerging evidence suggests that early exposure to endoscopic tools and procedures may also enhance medical student understanding of the field and stimulate career interest.¹⁰-¹²

With this in mind, the event began with an overview of gastroenterology as a specialty, including the training pathway into GI fellowship and the wide range of clinical and procedural opportunities within the field. Students then applied this knowledge through direct practice on an endoscopy simulator, gaining foundational skills and a deeper appreciation for this vital area of patient care.
In the endoscopy suite, gastroenterologists rely on strong interdisciplinary collaboration among anesthesia providers, nurses and endoscopy technicians. In alignment with osteopathic principles emphasizing teamwork and whole-person care, the interest group sought to foster the same spirit of cooperation and community. This commitment to collaboration was central to the success of the inaugural event and will continue to guide future opportunities for student engagement in gastroenterology.
After gaining early exposure to gastroenterology through a summer observership at AdventHealth Orlando and experiencing the value of endoscopy simulation firsthand, GI Interest Group President Juliana Madej was motivated to bring a similar opportunity to the ICOM campus. Alongside Vice President Hagen Shults, Secretary Allison Gronli and Treasurer Murali Bollampally, the leadership team collaboratively designed and coordinated this educational experience for their peers. In preparation, the team developed a foundational understanding of endoscope mechanics and instrumentation, enabling them to guide participants throughout the simulation while remaining adaptable to student needs during the event.
Student engagement was evident as participants enthusiastically navigated the Mikoto Colonoscopy Model using the endoscope. This hands-on experience allowed students to appreciate both the technical precision required in endoscopic practice and the ergonomic challenges that may arise during procedural work.
Notably, ICOM Dean Kevin Wilson, DO, FACOI, FACP, an internal medicine physician, also participated in the event, offering guidance and encouragement as students practiced maneuvering the scope.
In keeping with the Osteopathic Oath’s call to dedicate time and energy to the teaching of others, events such as this serve as meaningful opportunities to inspire exploration, mentorship and professional growth among medical students.
Osteopathic medical students remain underrepresented in gastroenterology, and increased early exposure and mentorship may be essential to strengthening the GI training pipeline. Initiatives such as endoscopy simulation events can help spark interest in subspecialty medicine while highlighting the diversity of career paths available within medicine.
Special Thanks to:
- Conor Broom, Fujifilm Endoscopy Account Executive
- Dr. Kevin Wilson, Dean and Chief Academic Officer of ICOM
- Dr. Jenifer Barry, GI Interest Group Faculty Advisor and Assistant Professor of Internal Medicine, ICOM
- Sharon Eisenbarth, Director of Student Affairs, ICOM
- ICOM Simulation Department
- ICOM Campus Security & Facilities Department
- ICOM Communications & Marketing Team
- Student Volunteers: Jonathan Shipp (OMS II), Hannah Farley (OMS II), Alexander Zaragoza (OMS II)
To stay connected and learn about future events, students and community members are encouraged to follow the ICOM Gastroenterology Interest Group on social media: Instagram @icom_gastro and X @icom_gastro.
References:
1. Silvestre J, Singh GP, DeLisser HM. Trends in Supply and Demand for Gastroenterology Training in the United States. Gastroenterology. 2023;165(4):819-824. doi:10.1053/j.gastro.2023.07.016
2. Kumar NL. Gastroenterology Fellowship Match: An Inside Look. Dig Dis Sci. 2018;63(3):545-546. doi:10.1007/s10620-018-4907-9
3. Teitelbaum HS, Ehrlich N, Travis L. Factors Affecting Specialty Choice Among Osteopathic Medical Students. Acad Med. 2009;84(6):718. doi:10.1097/ACM.0b013e3181a43c60
4. Brazdzionis J, Savla P, Oppenheim R, et al. Comparison of Osteopathic (DO) and Allopathic (MD) Candidates Matching Into Selected Surgical Subspecialties. Cureus. 15(6):e40566. doi:10.7759/cureus.40566
5. Qureshi UA, Yau A, Gutowski KS, et al. The impact of surgical elective exposure during medical school upon residency match rates. Heliyon. 2024;10(9):e29844. doi:10.1016/j.heliyon.2024.e29844
6. Atsawarungruangkit A, Chenbhanich J, Phupitakphol T, Dickstein G. Landing a GI Fellowship: The Match and the Map. Dig Dis Sci. 2018;63(3):605-609. doi:10.1007/s10620-017-4826-1
7. Raheel A, Dalla S, Birney J, et al. Interactive multidisciplinary pilot workshop to improve medical student perception of and interest in breast surgical oncology. The Breast. 2024;74:103690. doi:10.1016/j.breast.2024.103690
8. George J, Combellack T, Lopez-Marco A, et al. Winning Hearts and Minds: Inspiring Medical Students into Cardiothoracic Surgery Through Highly Interactive Workshops. J Surg Educ. 2017;74(2):372-376. doi:10.1016/j.jsurg.2016.10.002
9. Redepenning DH, Chau J, Dorris CS, et al. Scoping Review of Interventions and Experiences Increasing Medical Student Interest in Physical Medicine and Rehabilitation. Am J Phys Med Rehabil. 2023;102(3):275. doi:10.1097/PHM.0000000000002148
10. Persad AR, Verma LK, Persad R. Endoscopy simulation for pre-clerkship students. Can Med Educ J. 2020;11(1):e141-e143. doi:10.36834/cmej.67898
11. Finocchiaro M, Cortegoso Valdivia P, Hernansanz A, et al. Training Simulators for Gastrointestinal Endoscopy: Current and Future Perspectives. Cancers. 2021;13(6):1427. doi:10.3390/cancers13061427
12. Falon J, Brodaric AM, Whereat S, Storey D. Simulation of gastroscopy and endoscopic retrograde cholangiopancreatography for medical student education. ANZ J Surg. 2025;95(5):985-990. doi:10.1111/ans.19345
